AYIT Part 3: Maternal Mortality in the Late Victorian and Early Edwardian period
Introduction
In part 2, we looked at the state of midwifery in the United Kingdom in the nineteenth century, a practice that was being hamstrung by both the tripartite of the medical profession and by contemporary attitudes towards women. In this article we are going to take a look at the subject of maternal mortality, with specific reference to the years 1889 and 1890 when our cohort, who are the central theme of this series of articles, would have been born. One of the more famous names born in this period, who grew up not knowing their mother, was the artist Edward Alexander Wadsworth (b. 29 October 1889) who was closely associated with vorticism and known for his work on Dazzle camouflage for the Royal Navy.
For the year 1889, the maternal death rate for England and Wales was around 5.4 per thousand, or roughly 1 in 200, 0.5 percent. That might not sound particularly high, but if we look at the graph below, the figure remained constant since 1855 and it was not until 1930s that the number began to drop. There is a note about the data below, but there is a misconception that before the industrial revolution, there was a 'golden age' of natural childbirth — data is almost non-existent before the mid-19th century, but numbers are estimated to have been between 5 and 29 per thousand.1 While initially the figure of 1 in 200 sounds low, considering it happened consistently year on year (reflected in the flat line of the chart), it is high enough that people would have known friends, acquaintances, relatives or neighbours who had died as a result of child birth. The Church of England prayer book included a specific service for women who had recently given birth which began with the following line:
The safe deliverance and preservation from the great dangers of childbirth.2
This situation was not unique to the United Kingdom, and across America and Europe there were equally worrying rates, until developments in the 1930s (discussed below).3 In addition, maternal mortality mainly affected fit, young, healthy women regardless of their social background.4
The Numbers
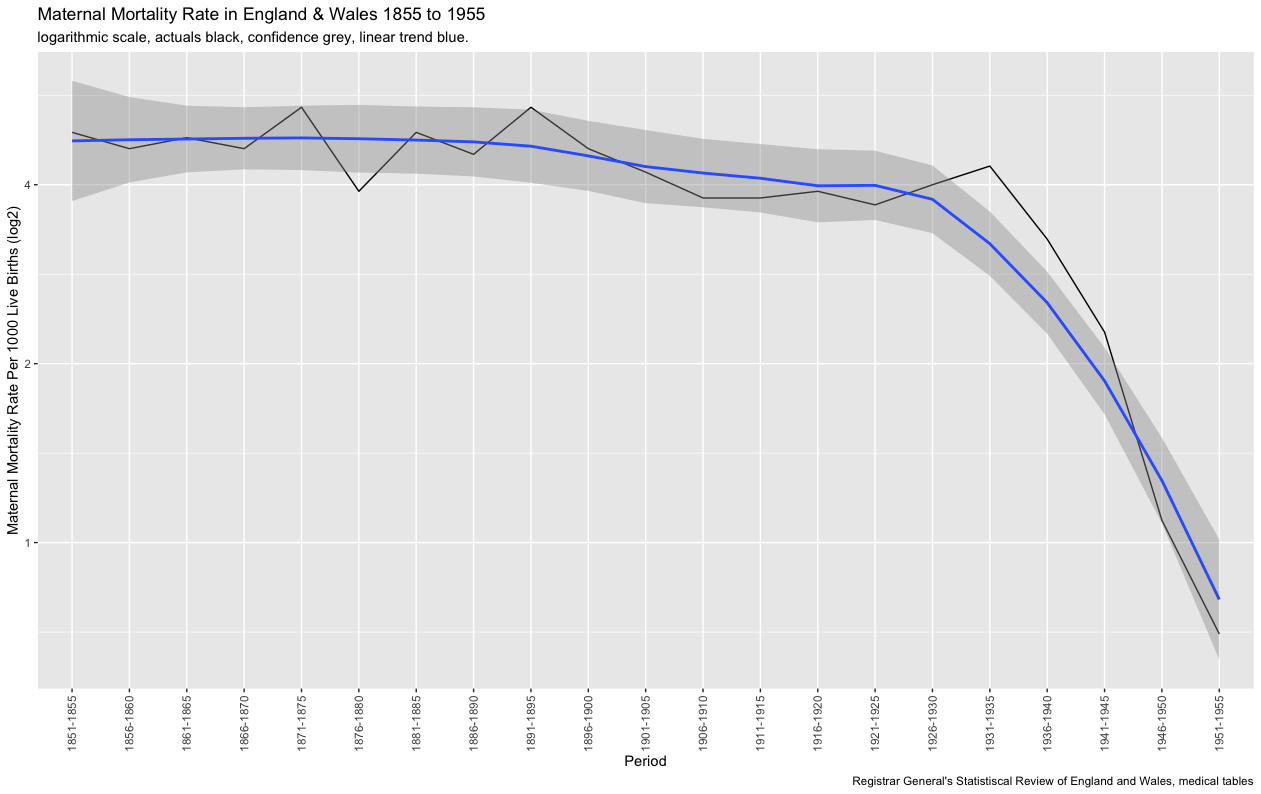
Figure . Maternal Mortality Rates in England and Wales 1855-1955
There are a few considerations to bear in mind regarding the figures used throughout this article. The first is that changes to recordkeeping practices during the period means there are both regional and chronological variances in the numbers.5 Secondly, the numbers were most certainly 'massaged' at times — the Rotunda Lying-in hospital in Dublin, for example, underreported maternal deaths to protect both reputations and income.6 There were, however, a number of groups and individuals concerned with the situation, such as epidemiologist and one of the founders of medical statistics Dr William Farr who, in a letter to the Registrar General in 1875, wrote: 'How long is this sacrifice of lives to go on?' Thus, there were several, sometimes quite detailed, studies undertaken which can be used to establish a clearer picture around the figures involved.7
The figure of 5.4 per thousand deaths for the year 1889 is the national figure. The numbers were as high as 8.1 in the Pontypridd district in Wales, and as low as 1.9 in Herford.8 In Lying-in hospitals, such as the aforementioned Rotunda, rates were much higher, though they were falling — the figure for Rotunda being 8 per thousand in 1889 from a high of 35 per thousand ten years earlier.9 To put Lying-in hospitals into perspective, in 1890 only 2,700 deliveries (0.3 % of all births) took place in the voluntary hospital sector, 1 percent took place in poor law hospitals and 4.6 percent under the care of dispensaries and Lying-in charities. Over 90 percent were home deliveries.10
Puerperal Fever
Approximately half of all maternal deaths were caused by puerperal fever, or puerperal pyrexia as it is known today, a bacterial infection which normally ended with one of three outcomes: a localised pelvic abscess which the body could, in most cases, fight off; a septic thrombophlebitis in the pelvic veins which was usually fatal; and peritonitis - where the bacteria spread to the fallopian tubes, leading to a painful death. Puerperal fever did not care if its host was rich or poor and as mentioned in the introduction, deaths occurred in mostly healthy young women.11 Unhygienic practices, such as the doctor or midwife using a communal pot of hog's lard to lubricate their fingers, as happened at the Rotunda Hospital, undoubtedly contributed to the higher incidence of puerperal fever in Lying-in hospitals.12 There were a number of old wives tales in existence, relating to home births, such as that death could be avoided if the recent mother wore her stained underclothes for a week after the birth.13 Puerperal fever could also be spread via midwives going from home to home and there are several accounts in the newspapers of this happening, suggesting it was quite a common occurrence.14 It also seemed to be especially problematic in the Rhonda valley, and remained so well into the start of the 20th century. The medical officer for health in 1900 reported:
It is extremely difficult to get the class of women who usually act as monthly nurses to realise the need for cleanliness in their work. In one instance a woman was attending cases while she was living in a house where there was a virulent case of diphtheria; it is little wonder, therefore, that her patients were attacked with puerperal fever. At first she obstinately refused to go to the hospital, but when I saw her and saw the condition of her surroundings, and of her clothing, and the little attention she had given to personal cleanliness, I felt justified in taking the most extreme steps to prevent her attending any more patients as she then was.15
In the previous article, I highlighted the elitism that existed within the medical tripartite, in particular how they treated and viewed women, but this elitism didn't stop there. This was a major issue across the developed world. The establishment belief was that the fever was spread through vapours in the air that mysteriously transferred from woman to woman.16 It took the best part of a century for the profession to come around to the fact that it was transmitted by birth attendants and propagated by poor hygiene. Three individuals did make the connection early on and deserve a mention here. The first was Alexander Gordon (1752-1799), a naval surgeon who while on half-pay leave, working at an Aberdeen institute in 1790 during an epidemic of puerperal fever, made the connection between the disease being spread via doctors and nurses and dirty bedclothes. His reward was being hounded from Aberdeen and back into the navy. Oliver Wendell-Holmes (1809-1894), an American physician, also made the connection between the disease being spread via doctors and nurses and he too was vilified by the medical profession. Hungarian Physician Ignaz Semmelweis (1818-1865), who proved that washing hands before attending to women in labour greatly reduced incidences of disease, and published the Aetiology of Childbed fever in 1858, was also highly ostracised by the profession across Europe. There was great resistance and denial of these three people's claim, because accepting the conclusions of Gordon, Holmes and Semmelweis meant the profession would have to accept the fact they were in the wrong, and that they and their colleagues were responsible for taking lives, rather than saving them.17
It was not until 1879 that the French chemist and father of modern bacteriology Louis Pasteur (1822-1895) showed that streptococcus, a type of bacteria, could be cultured from most cases of puerperal fever. Inspired by Pasteur's work on 'germ theory', the surgeon Joseph Lister (1827-1912), working at the Royal Infirmary in Glasgow, came up with the use of a carbolic spray to sterilize instruments and bandages (antisepsis). In 1880, Lister moved to Kings College, London where he introduced his system to the General Lying-in Hospital, a major venue for the training of midwives, which began to bring down the high-rates within Lying-in hospitals across the country over the course of the decade.18 This, along with the uptake of asepsis — the keeping of bacteria away from wounds via better hygienic practice — began to bring the number of deaths down further, although it was not until the 1920s that the British College of Obstetricians recommended the use of facemasks and not until 1929 the use of rubber gloves.19 The biggest factor in the decline of puerperal sepsis, however, would not come about until 1936 with the discovery of sulphonamides, an antibiotic, alongside parallel improvements in education, clinical care, blood transfusion, and better nutritional and antenatal care, to name a few, when the death rate was brought down to less than 44 in 100,000, as it stands in the UK today.20
Other Causes
Medical literature of the 19th century devoted many pages to the subject of obstructed labour, and here the health of the mother certainly played a part. For example, Glasgow in 1889 was at the tail-end of a rickets epidemic, which made the likelihood of an obstructed pregnancy much greater. At the time, the understanding of rickets as a separate disease from scurvy was still in its infancy. A connection to poor diet had been made, but it would be another 30 years before the link between vitamin D deficiency and the disease would become clear. Interestingly, Leonard Findlay (1878-1947), a physician with the Royal Hospital for Sick Children, was convinced the answer to rickets lay with fresh air and exercise, not realising that it was the sun and its concomitant ultraviolet light that caused the improvements in his patients — a classic case of misinterpretation of the evidence.21 Though it filled pages of the medical texts, obstructed labour was not actually very common. The high wordcounts devoted to the subject reflected the midwives' and surgeons' fear of obstructed labour rather than the reality; while caesarean sections dated to Roman times, it was a risky practice and was rarely employed until the 1930s.
The next largest causes of maternal mortality, accounting for a quarter of all deaths, was down to ante- and post-natal haemorrhage, and toxaemia.22 Toxaemia, pre-eclampsia and eclampsia are difficult to surmise as they were unknown conditions at the time. Deaths were recorded as being either down to fits or renal failure, mainly in younger women.23 The cause for these conditions are also not well understood today, but the evidence suggests that occurrences of toxaemia were no more common back then than they are now.24 A change has come about in the management and early diagnosis of risk, through the regular monitoring of blood pressure and the introduction of a national system of antenatal clinics, introduced by physician and medical officer Janet Campbell (1877-1957) in the 1920s.25
Regarding haemorrhages, which tended to affect older women, again there is difficulty in trying to surmise such outcomes due to regional differences. An observation by medical historian Irvine Loudon is that both Toxaemia and ante-natal haemorrhage were higher in women of a higher social class than those of the lower classes, and post-natal haemorrhage was higher in lower classes than in the upper.26 The reason for this needs to be treated with care as the analysis relies on hindsight. In the previous articles, I mentioned complaints about male practitioners of the time being impatient, accusations of unnecessary interferences and the overzealous use of forceps — this comes through in the evidence. A study of child deliveries undertaken in Wales showed that in deliveries where there was just a midwife, the use of forceps in general was around three to five percent, however where the general practitioner was called in, the rate was as high as 56%.27 Evidence also seems to suggest that where there was a general practitioner present, there was a better chance of surviving post-natal haemorrhage than if there had just been a midwife. To step back for a moment, for context, the numbers we are talking about here are a fraction of a percent of all births and the aforementioned is a very small proportion of that fraction. The health of the mother, especially good nutritional health, was pivotal in not only reducing the risk of haemorrhage but the likelihood of a healthy delivery — it would not be until the 1930s before this was better understood.28 Both ante- and post-natal haemorrhage deaths were greatly reduced by improvements in education, training, and developments in the process of blood transfusion. The synthesis of the peptide oxytocin in the 1950s, a synthetic version of the peptide of the same name, which stops bleeding following delivery, meant that in the developed world, blood loss as a cause of maternal death was almost eradicated.29
There was one other major cause of maternal mortality — abortion. As this series of articles is interested in society, this topic deserves its own post, especially to investigate attitudes of the time, and there are a few other topics, such as the Edwardian crisis, that I want to cover first, to provide a framework for context. It is worth noting, however, that most abortions undertaken at the start of the period under investigation where were sought by married women in their late 30s and 40s in cases where contraception had failed.30
Summary
I mentioned in part two that there is a lazy narrative that blames the Industrial Revolution, overcrowding and poverty for the high mortality rates of the time. I hope providing more rigorous analysis here, along with the previous article, has given some insight to why that narrative is spurious. I will start to take it apart further in part 4 when looking at infant mortality. If such a narrative was true there would be correlation between maternal and infant mortality, and — spoiler alert — there isn't.
The main takeaway for myself from researching this topic, is that today we speak about health and other matters in the United Kingdom as a 'postcode lottery', and while it is an anachronism when applied to the 19th century (as postcodes were first introduced in 1959), where you were born, regardless of class, represented a roll of the dice for your health, but with one crucial difference. While there was national awareness of issues such as puerperal fever, I don't believe many people of the time, would have been aware of for, example, those observations made by Loudon noted above — much of the analysis from the sources used throughout this article is comes from a position of hindsight. Society was focused far more locally that it is today, a topic we will be returning to often throughout these articles; part two mentioned that midwives and general practitioners relied on word-of-mouth recommendations, thus the immediate social circle around the mother of the time would had played a part in the decisions made about giving birth. Without awareness of the national picture, I would go as far to say that, if X was the midwife for the village and they had a higher-than-average mortality rate, it would be accepted as 'that was the way things were'. Finally, the fear of death in childbirth was very real, for good reason but, as later articles will show, this was just one of many fears of death our cohort would experience.
-
Edward Wadsworth, https://spartacus-educational.com/ARTwadsworth.htm , viewed on 14 March 2022. ↩︎
-
Quoted in, G. Chamberlain, 'British Maternal Mortality in the 19th and Early 20th Centuries', Journal of the Royal Society of Medicine, 99(11) (2006), p.559. ↩︎
-
I. Loudon, 'Maternal mortality in the past and its relevance to developing countries today', American Journal of Clinical Nutrition, 72(1) (2000), p.24. ↩︎
-
Chamberlain, 'British Maternal Mortality', p.559. ↩︎
-
Chamberlain, 'British Maternal Mortality', p.559. ↩︎
-
J.A. Bergin, 'Birth and Death in Nineteenth-Century Dublin's Lying-in hospitals' in Farrell (ed.), She said she was in the family way (London: University of London Press: Institute of Historical Research, 2012), pp.107-108. For Scotland see also: A. Reid, E. Garrett, 'Medical Provision and Urban-rural Difference in Maternal Mortality in Late Nineteenth Century Scotland', Social Science & Medicine, 201 (35-43) (2018). ↩︎
-
I. Loudon, 'Deaths in Childbed from the Eighteenth Century to 1935', Medical History, 30(1) (1986), p.2. ↩︎
-
E. Macdonald, 'A Slave to the Home: Female Labour and Mortality in the Rhondda; 1881-1911 (Student Dissertation for the Open University module A329 The Making of Welsh History, 2019), p.13. ↩︎
-
Bergin, 'Birth and Death', pp.107-109. ↩︎
-
Loudon, 'Deaths in Childbed', p.22. ↩︎
-
Chamberlain, 'British Maternal Mortality'p.559. ↩︎
-
J Bergin, 'Birth and Death', pp.107-97. ↩︎
-
S. Meacham, A Life Apart: The English Working Class 1890-1914 (London: Thames and Hudson, 1977), p.70. ↩︎
-
For example, see: Leeds Times - Saturday 21 September 1889; Berks and Oxon Advertiser - Friday 06 December 1889. ↩︎
-
Lisa Jane Snook, 'Women in Rhonda Society, c,1870-1839' (PhD, Swansea University, 2002), pp.155-156. ↩︎
-
Chamberlain, 'British Maternal Mortality', p.560. ↩︎
-
Chamberlain, 'British Maternal Mortality', p.560. ↩︎
-
Helen Joan Betts, 'A Biographical Investigation of the Nightingale School for Midwives (PhD, University of Southampton, 2002), p.70. ↩︎
-
Chamberlain, 'British Maternal Mortality', pp.561-562. ↩︎
-
Loudon, 'Deaths in Childbed', p.41. ↩︎
-
G. C. Arneil, 'Nutritional rickets in children in Glasgow', Proceedings of the Nutrition Society. Cambridge University Press, 34(2) (1975), pp.101-102. ↩︎
-
Loudon, 'Deaths in Childbed', p.22. ↩︎
-
Chamberlain, 'British Maternal Mortality', p.562. ↩︎
-
Loudon, 'Deaths in Childbed', p.23. ↩︎
-
Chamberlain, 'British Maternal Mortality', p.562. ↩︎
-
Loudon, 'Deaths in Childbed', p.35. ↩︎
-
Loudon, 'Deaths in Childbed', p.36. ↩︎
-
Loudon, 'Deaths in Childbed', p.36. ↩︎
-
Chamberlain, 'British Maternal Mortality', pp.562. ↩︎
-
Chamberlain, 'British Maternal Mortality', pp.562. ↩︎
Posts in this Series
- AYIT Part 4: An overview of Infant Mortality in England and Wales: 1870-1910
- AYIT Part 3: Maternal Mortality in the Late Victorian and Early Edwardian period
- AYIT Part 2: A Brief Overview of the state of Midwifery in the 1800s
- AYIT Appendix 1.1: Voluntary Maternity Hospitals 1860-1930
- Are YOU in this ? Bibliography
- Are YOU in this ? Part 1: An Introduction