AYIT Part 2: A Brief Overview of the state of Midwifery in the 1800s

Martha used to come, the midwife. She wasn't certified or anything, but she was one of the good old midwives and it was only a few shillings for a confinement. I've heard m'mother say that she used to give her sixpence a week until she got paid off. She was a grand old lass. In George Street that was.1
In the introduction, our cohort were introduced as being approximately 1.1 million in size based on the number of births recorded across the United Kingdom between 5 August 1888 and 4 August 1889. In 1889, the infant mortality rate was approximately one in seven, which means our cohort would have decreased by 159,000 — equivalent to the entire population of Cambridge in 2011.2 Maternal mortality rates were around one in two hundred, high enough for expectant mothers to fear the prospect, with some writing a testament of sorts to their existing or coming child, afraid that, should they die, their memory would be lost — especially if the husband was to remarry.3 Both maternal and infant mortality rates varied around the UK, with the risk of dying from childbirth being higher in the north, while infant mortality rates were higher in urban areas.4 The lazy answer to why both rates were so high blamed 'industrialisation, poverty and something about overcrowding'. Given that the 'health of the nation' forms an important part of the narrative of the First World War in the first few articles of this series, we will be examining why such an answer is far too simplistic. We start with an overview of midwifery in the 1800s and follow this with a detailed look at both maternal and infant mortality in the next two articles, ending with a look at the advice published in midwife manuals of the time. The reason for providing an overview is twofold: our period cuts through an intriguing chapter of the history of midwifery (roughly 1750-1950), in the twilight era before public hospitals and national health against a backdrop of a period of discovery and change; and the conclusion we cut through to says a lot about the society our cohort is about to enter.
Up until the 1730s, midwifery was carried out almost exclusively by women. They were known as 'handy women', 'helper outers' and in one case, in County Wexford, as the 'rabbit catcher'.5 In Scotland they were known by other names, such as 'skilly', 'neighbour women' and the most common 'howdie'.6 One of the most important and skilled of the time was Sarah Stone of Taunton, Somerset, who in 1737 would write the enlightened treatise A Complete Practice of Midwifery based on her 35 years' experience. Having learnt her craft from being apprenticed to her mother for six years, at the peak of her career she was overseeing some 300 births a year and was often called in as a consultant for difficult births.7 Between 1730 and 1800 the number of medical men practicing midwifery shot up exponentially. While the reason for this increase is still up for debate, the traditional explanation is 'Fashion and Forceps' with surgery becoming more popular and the discovery of the forceps in 1730 providing a powerful tool for the medicine man. The late medical historian Irvine Loudon argues that it was more to do with the new spirit of enquiry into fields of anatomy and physiology, and the rise of rank-and-file practitioners, later to be known as general practitioners, who saw man-midwifery as a good source of additional income and a good way to expand and grow their practices.8 In parallel to this development, the 1700s saw the introduction of the lying-in hospitals, the first to be dedicated to care of parturient women, in Scotland, England and Ireland — but curiously not Wales.9 Both factors would play a role in diminishing the formal status of the female midwives traditionally seen as independent experts, who by the 1870s had led to some contemporary commentators to place them 'below the class of the ordinary domestic servants'.10 While reputations improved in the latter part of the 1800s, it would not be until the passing of the 1902 Midwives Act that the previous status quo would be returned to. Before the passing of the Act, it was perfectly possible for anybody, male or female, to refer to themselves and operate as a midwife. Shops such as E & R Garrould, Edgware Road, London would sell you everything you needed, from uniforms and books to surgical instruments.11 Bear in mind, however, that most midwives were employed based on their reputations and through personal recommendations.12
The medical profession
At the start of the 1800s, the medical men had gained a monopoly on midwifery partly due to the disdain shown by the traditional tripartite of the medical profession: physic, surgery, and pharmacy. The College of Physicians asserted that their role was in the care of women before and after labour, but not during it. The newly established (in 1800) Royal College of Surgeons held both the practice of midwifery and pharmacy in contempt, going so far in their elitist approach to exclude from the college those who practiced these disciplines. The Society of Apothecaries ended up initially attempting to administrate midwifery, but as they were essentially a wholesale drug company, they were the least suited to do so and they did not have the legal authority to act.13 In response to the inertia shown by the tripartite, the physician A.B. Granville established the Obstetrical Society in 1825 with the aim to 'raise to a proper dignified status to the practician of midwifery', and to procure by legislation the regulation of the obstetric profession, for both male and female. While its plans were ambitious and it found favour with medical practitioners and the Home Secretary, the Society would fade away by 1830 due to the 'intellectual arrogance' shown by the higher echelons of the medical profession.14 Whilst surgeons and physicians were seen as socially acceptable, obstetrics was seen as an 'extra' not worthy of the time of those devoted to the study of physic, surgery and medicine — this was an attitude that would remain for much of the 1800s.15 It was therefore the general practitioners who would fill the void and, seeing both the traditional female midwife and any attempts to train and regulate her as competition to their own practices, they became outwardly hostile towards them, painting midwifes as incompetent, dangerous and unscientific.16 Sairey Gamp — the drunk and sloppy nurse in the Charles Dickens novel Martin Chuzzlewit — became a common slur used amongst doctors.17 Medical literature of the time is full of antipathy towards bona fide midwives — much of this rhetoric was, however, anecdotal.18 The surgeon Henry Bott, giving evidence to the 1893 Select Committee, attacked unqualified midwives, but when asked to provide evidence he was unable to do so, except to say he had 'many cases of suspicions'.19 The doctors themselves were not free from criticism either: common complaints included being impatient, the overuse of forceps in examinations, and accusations of unnecessary interference. Dr Cameron of Glasgow informed the 1892 Select Committee that: 'A chapter of horrors might easily be written upon the mismanagement of labour, in which only the mystic letters appended to the operator's name protected him from prosecution'.20
Female Midwives
Turning our attention back to female midwives, the practice itself became hierarchical, with those working at lying-in hospitals looking down on the unqualified bona fide midwife. A new category of nurse emerged known as a monthly nurse (sometimes incorrectly referred to as a midwife) who trained at lying-in hospitals not to deliver babies, but to take care of women before and after labour. In a time of contradictions, they were not highly thought of in the public sphere but were admired by accoucheurs and a good monthly nurse often found herself in the employment of one so that he did not have to be present throughout the entire labour — under the threat of dismissal if she did fail to call the doctor in when birth was imminent.21 It is important to note at this juncture that much of what has been said relates to a small part of society; the majority of deliveries carried on in the home and, regardless of whether a male or female midwife was present, it was reputations rather than certifications or training that mattered when it came to employment.22 In rural and traditional communities, many of the old customs persisted and there were a number of successful and respected 'unqualified midwives', such as Mary Eaves in Coventry who, between 1847 and 1893, oversaw some 200 deliveries a year.23 As successful as they were, the future of midwifery would remain in the hands of the few. The bona fide midwife lacked the voice and unity to take on the establishment and it is hard to ascertain if people such as Mary Eaves were even aware of the debate surrounding the profession.24
In the 1850s, attitudes began to change — slowly. The Royal College of Surgeons introduced a diploma in midwifery in 1852 for men. When three women — Sophia Jex-Blake, Miss Thorne, and Miss Pechey — applied to take the examination in 1872 the examiners resigned.25 In 1858 the Obstetrical Society of London was inaugurated because, like its previous namesake, of what it saw as the inactivity of the tripartite.26 In 1872, the organisation began issuing certificates of competence to midwives, however they were controversial due to only covering 'natural labours' and midwives were expected to refer to an obstetrician in case of difficulties.27 In 1875, the General Medical Council discussed suggestions to allow women to pursue medical practice on the same footing as men, which they dismissed due to women not possessing 'the peculiar moral and physical qualities' required in a practitioner. There was, however, a small, albeit hollow victory. The Council noted
...[we] believe that a much more limited and less expensive Education might be afforded to Women who after due Examination might, as Midwives, render valuable service to the community...28
As historians Sarah Fox and Margaret Brazier point out in The Regulation of Midwives in England, c.1500-1902, most of the proposals put forward for regulation were concerned with the need for medical (and male) supervision, education, examination and registration. The examinations themselves were less to do with skill but more about the women's level of education and wealth.29 For example, the cost of midwife training in the 1880s was £10, putting it out of reach for most, and the London lying-in hospital charged between £30 and £50, a fee only the wealthiest of women could pay.30
Lying-in Hospitals & Campaigners
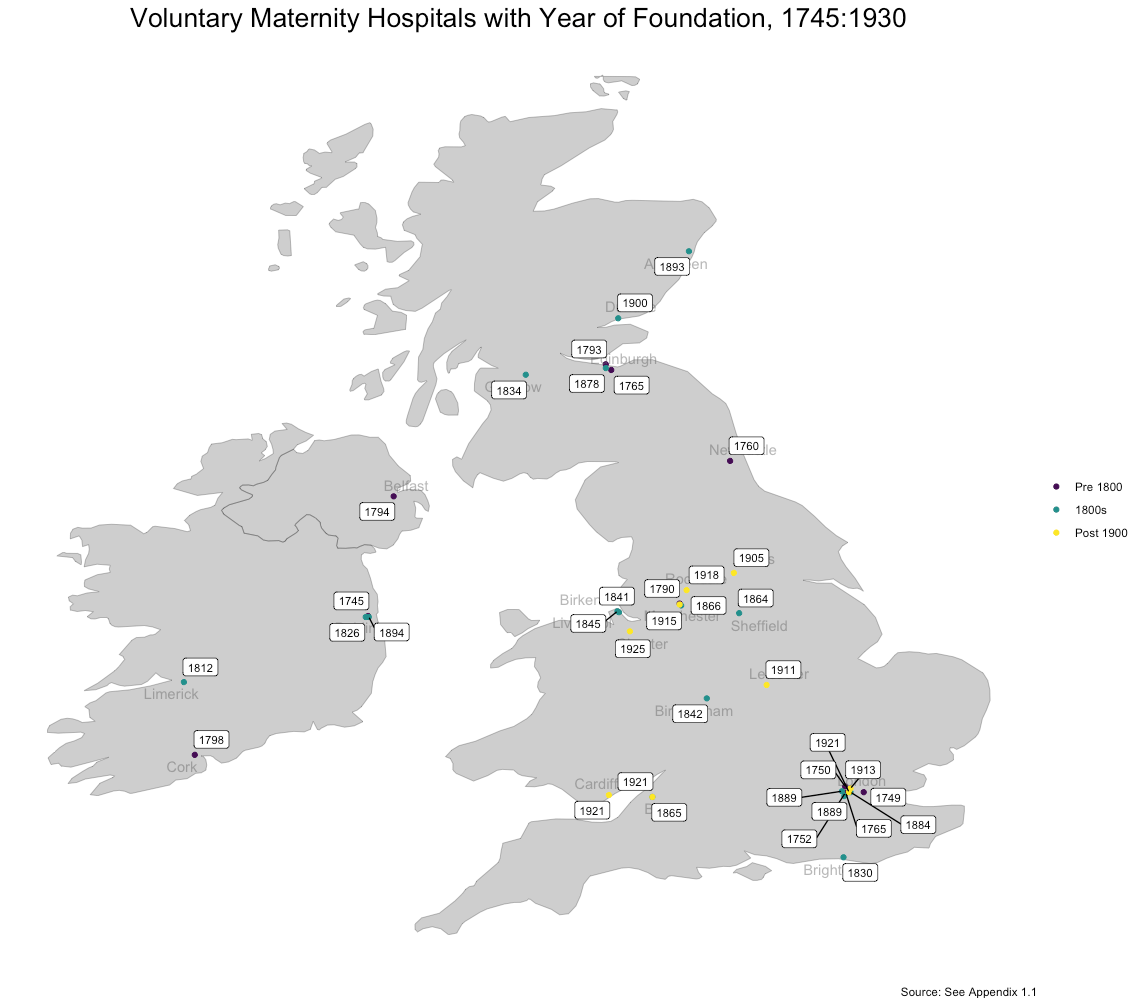
At the start of the 1800s there were just ten maternity hospitals throughout the British Isles and a further sixteen were added throughout the century.31 Without regulation or oversight, by the 1870s they had become the deadliest of places to give birth. Epidemiologist and one of the founders of medical statistics Dr William Farr remarked in 1875:
Seeing how destitute of comforts, means, and medical appliances many women are, the thought occurred to some benevolent person that they might be received and delivered in hospitals. It was the extension of the hospital system to midwifery cases, which have some analogy with wounds and injuries for which hospitals had been used from the date of their foundation. Contrary to expectations the advantages these institutions offered were over-balanced by one dread draw back; the mortality of mothers was not diminished; nay it became in some instances excessive; in other instances, appalling.32
The Queens Charlotte's Hospital in London, between 1857 and 1879, had an average maternal mortality rate of 29.6 per 1,000, reaching a high of 84.4 per 1,000 in 1859.33 This compared to a figure of just 2.9 per 1,000 for home births, which led to the Lancet beginning a campaign to question whether lying-in hospitals had the right to exist.34 In 1875 Farr himself wrote to the GMC: 'How long is this sacrifice of lives to go on?'35 There were growing numbers of campaigners from all quarters trying to address the growing problems around childbirth. Among them were Florence Nightingale — campaigning for better training of nurses — who started her own school of midwifery at Kings College London in 1862;36 and Dr James Edmunds, who wanted to detach midwifery from medical practice and save women from the distress of male attendants.37 The Ladies Medical College was formed in 1861, which Nightingale recognised as producing some of the best trained midwives in the country, and had wide support including from William Farr and prominent individuals such as Lord Shaftsbury.38 In the 1880s a group of diploma-holding midwifes set up the Midwives Institute with the aim to gain legislation and regulation of midwifery by putting pressure on the government.39 By 1889 and 1890, both the Lancet and the GMC had added to the pressure building on the government to act.40 1891 would also see the Obstetrics society come up with a certificate for women — though it had no legal basis, it did gain a lot of respect from male medical practitioners adding weight to the midwives' call.41 All the momentum building up in the last two decades of the 1800s eventually led to the passing of the 1902 Midwives Act. There is one last 'however', and this is the indicator of what society is like for the world our cohort are about to enter. It took six debates in the House of Commons between 1883 and 1902 before the Act passed. The debates were less about the skill and capability of midwives but were more concerned about giving women professional status.42
The 1902 act on its own did not solve the issues around high mortality rates, and it would take some years to see it effects filter through. While all parties involved during this period were acting in what they thought was in the best interest there was, in hindsight, an immense amount of ignorance displayed which will be examined in more detail when we look at maternal mortality rates in part three.
Image Credits
Figure 1. Photograph of Mrs McDonald, a midwife in Invercreran, Argyll,
c1866
National Records of Scotland, GD1/1208/1/52 , used under Open
Government Licence
Information
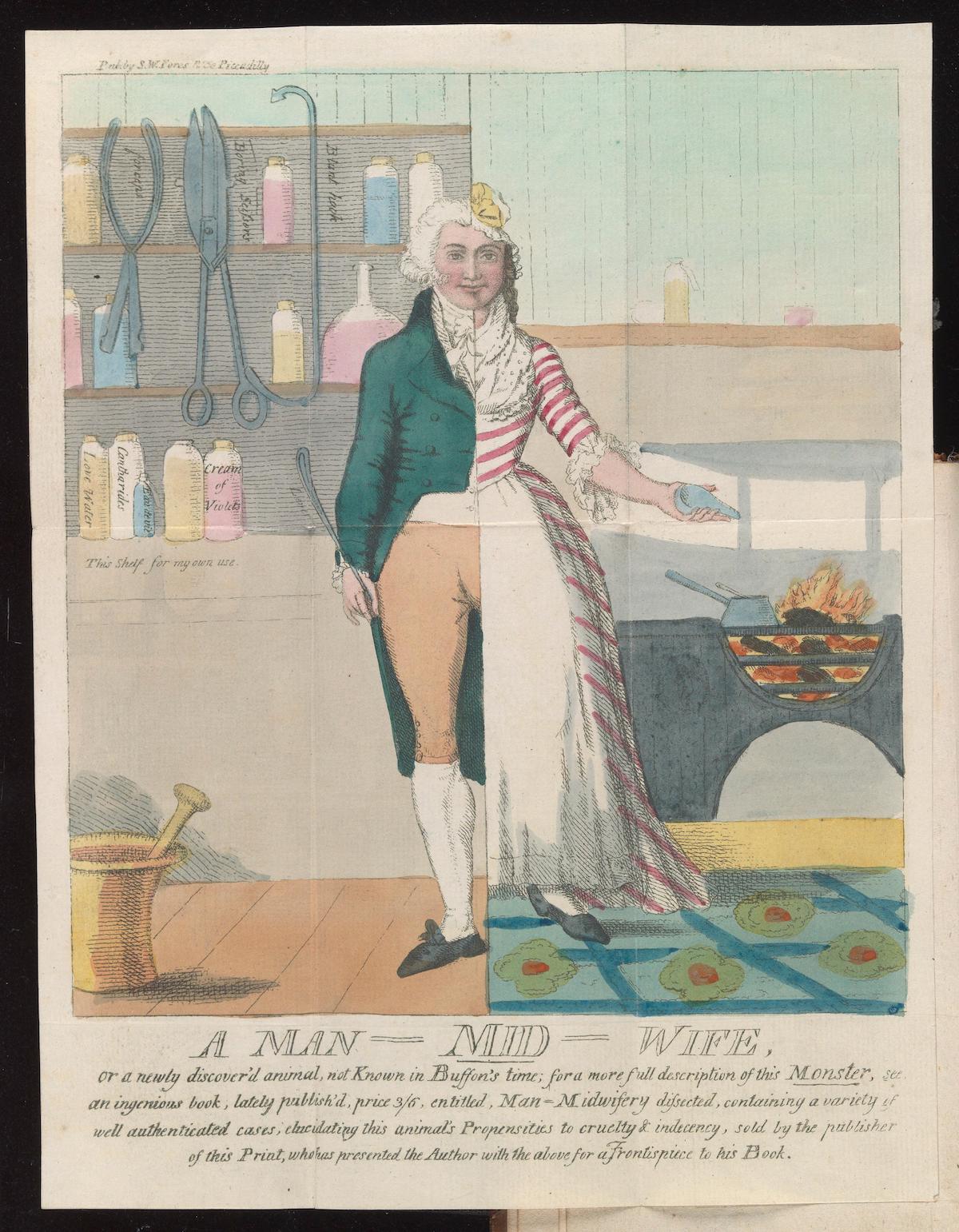
Figure 2. Man-midwifery dissected; or, the obstetric family-instructor: In fourteen letters. Addressed to A. Hamilton. Occasioned by certain doctrines contained in his letters to Dr. W. Osborn / By John Blunt [i.e. S.W. Fores]. Credit: [Wellcome Collection]{.ul}. [Public Domain Mark]{.ul}
-
Mrs Harte, born in Lancaster in 1889, whose mother had eleven births. Quoted in, L. M. Beir, 'Expertise and Control: Childbearing in Three Twentieth-Century Working-Class Lancashire Communities', Bulletin of the History of Medicine, 78(2) (2004), p.400. ↩︎
-
Office for National Statistics; National Records of Scotland; Northern Ireland Statistics and Research Agency (2017): 2011 Census aggregate data. UK Data Service (Edition: February 2017). ↩︎
-
P. Kane, Victorian Families in Fact and Fiction (New York: St Martin's Press, 1997[1995]), p.129. ↩︎
-
I. Loudon, 'Deaths in Childbed from the Eighteenth Century to 1935', Medical History, 30(1) (1986), p.2. ↩︎
-
J.A. Bergin, 'Birth and Death in Nineteenth-century Dublin's Lying-in Hospitals' in Farrell (ed.), She said She was in the Family Way (London: University of London Press: Institute of Historical Research, 2012), p.99. ↩︎
-
'Safe Delivery: A History of Scottish Midwives', https://www.nrscotland.gov.uk/research/learning/features/safe-delivery-a-history-of-scottish-midwives, viewed 24 November 2021. ↩︎
-
A. Bosanquet, 'Sarah Stone: The Enlightenment Midwife', The Practising Midwife, 12(9) (2009), p.31. ↩︎
-
When forceps were first used in England is a mystery. The Chamberlains invented the obstetric forceps and kept it a secret for three generations before publishing the design in 1730. After this date they became widely known and used; I. Loudon, 'Deaths in Childbed', p.7, note. 12. ↩︎
-
A. J. Muir, 'Midwifery and Maternity Care for Single Mothers in Eighteenth-Century Wales', Social History of Medicine, 33(2), p.397. ↩︎
-
J.A. Bergin, 'Birth and Death', p.100. ↩︎
-
H. Morten, The Midwives Pocket Book (London: The Scientific Press, 1897) ↩︎
-
S. Fox & M. Brazier, 'The Regulation of Midwives in England, c.1500-102', Medical Law International, 20(4) (2020), p.328. ↩︎
-
I. Loudon, 'Deaths in Childbed', pp.10-11; S. Fox & M. Brazier, 'The Regulation of Midwives', p.330. ↩︎
-
D.I. Williams, 'The Obstetric Society of 1825', Medical History, (42) (2), pp.235-244. ↩︎
-
I. Loudon, 'Deaths in Childbed', pp.11-12. ↩︎
-
Helen Joan Betts, 'A Biographical Investigation of the Nightingale School for Midwives (Ph d, University of Southampton, 2002), p.58. ↩︎
-
I. Loudon, 'Deaths in Childbed', p.38. ↩︎
-
J.A. Bergin, 'Birth and Death', p.101. ↩︎
-
S. Fox & M. Brazier, 'The Regulation of Midwives', p.332. ↩︎
-
I. Loudon, 'Deaths in Childbed', 30(1) (1986), p.36. ↩︎
-
Betts, 'A Biographical Investigation', p.58; J.A. Bergin, 'Birth and Death', p.102. ↩︎
-
S. Fox & M. Brazier, 'The Regulation of Midwives', p.328. ↩︎
-
S. Fox & M. Brazier, 'The Regulation of Midwives',), p.331. ↩︎
-
F. J. Badger, 'Illuminating Nineteenth Century English Urban Midwifery: The Register of a Coventry Midwife', Women's History Review 23(5) (2014), p.698. ↩︎
-
I. Loudon, 'Deaths in Childbed', pp.11. ↩︎
-
D.I. Williams, 'The Obstetric Society of 1825', Medical History, (42) (2), p245. ↩︎
-
S. Fox & M. Brazier, 'The Regulation of Midwives', p.330. ↩︎
-
S. Fox & M. Brazier, 'The Regulation of Midwives', p.331. ↩︎
-
S. Fox & M. Brazier, 'The Regulation of Midwives', p.330. ↩︎
-
Betts, 'A Biographical Investigation', p.73. ↩︎
-
Craig Stephenson, 'The Voluntary Maternity Hospital: a Social History of Provincial Institutions, with special reference to maternal mortality, 1860-1930' (Ph D, University of Warwick, 1993), p.80. ↩︎
-
Quoted in I. Loudon, 'Deaths in Childbed', p.19. ↩︎
-
I. Loudon, 'Deaths in Childbed', p.21. ↩︎
-
Craig Stephenson, 'The Voluntary Maternity Hospital', p.82. ↩︎
-
I. Loudon, 'Deaths in Childbed', p.2. ↩︎
-
Betts, 'A Biographical Investigation', p.73. ↩︎
-
Betts, 'A Biographical Investigation', p.75. ↩︎
-
Betts, 'A Biographical Investigation', p.76. ↩︎
-
Betts, 'A Biographical Investigation', p.80. ↩︎
-
Betts, 'A Biographical Investigation', p.81. ↩︎
-
S. Fox & M. Brazier, 'The Regulation of Midwives', p.330. ↩︎
-
S. Fox & M. Brazier, 'The Regulation of Midwives', p.329. ↩︎
Posts in this series
- AYIT Part 4: An overview of Infant Mortality in England and Wales: 1870-1910
- AYIT Part 3: Maternal Mortality in the Late Victorian and Early Edwardian period
- AYIT Part 2: A Brief Overview of the state of Midwifery in the 1800s
- AYIT Appendix 1.1: Voluntary Maternity Hospitals 1860-1930
- Are YOU in this ? Bibliography
- Are YOU in this ? Part 1: An Introduction